Cross-posted at Family Inequality.
There’s an interesting example of how to interpret scientific results — and draw policy implications from them — from the world of birth practices and safety.
The subject of the debate is a major new study from the British Medical Journal. The study followed more than 60,000 women in England with uncomplicated pregnancies, excluding those who had planned caesarean sections and caesarean sections before the start of labor. They compared the number of bad outcomes — from death to broken clavicles – for women depending on where they had their births.
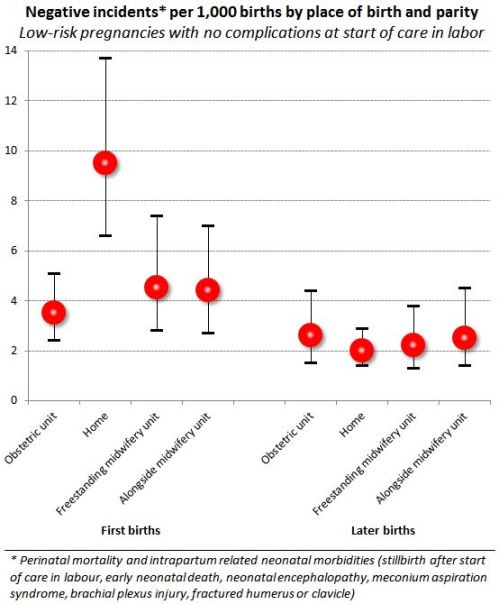
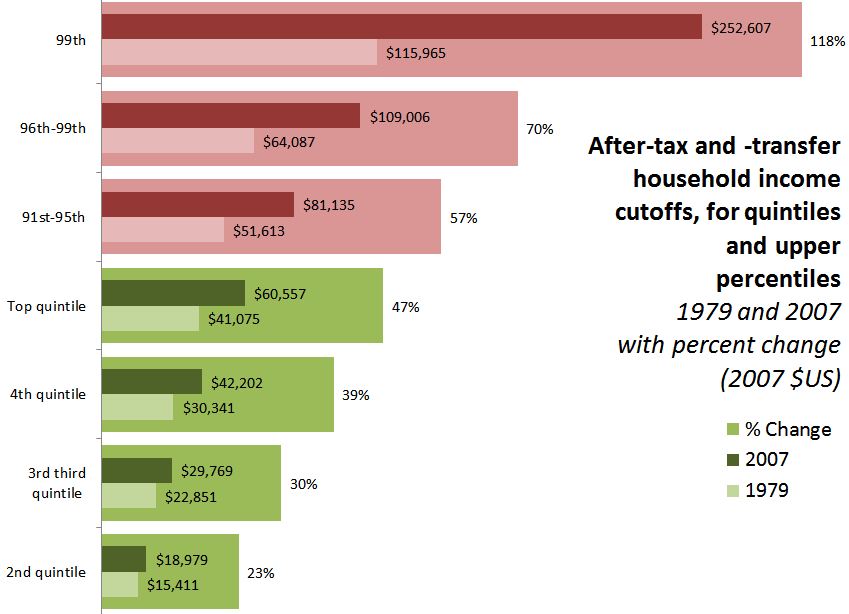
One comparison stands out in the results. From the abstract: “For nulliparous women [those having their first birth], the odds of the primary outcome [that is, any of the negative events] were higher for planned home births” than among those planned for delivery in obstetric units. That is, the home births had higher rates of negative events. The difference is large. Here’s a figure to illustrate:
The error bars show 95% confidence intervals, so you can see the difference between home births and obstetric-unit births is statistically significant at that level. These are the raw comparisons, but the home-versus-obstetric comparison was unchanged when the analysts controlled for age, ethnicity, understanding of English, marital or partner status, body mass index, “deprivation score,” previous pregnancies, and weeks of gestation. Further, by restricting the comparison to uncomplicated pregnancies and excluded all but last-minute c-sections, it seems to be a very strong result.
But what to make of it?
In their conclusion, the authors write:
Our results support a policy of offering healthy nulliparous and multiparous women with low risk pregnancies a choice of birth setting. Adverse perinatal outcomes are uncommon in all settings, while interventions during labour and birth are much less common for births planned in non-obstetric unit settings. For nulliparous women, there is some evidence that planning birth at home is associated with a higher risk of an adverse perinatal outcome.
But in what way do the results “support a policy”? The “higher risks” they found for planned home births are still “uncommon,” by comparison, with those in poor countries, for example. But the home birth risk is 2.7-times greater.
The Skeptical OB, who is a reliable proponent of modern medical births, titled her post, “It’s official: homebirth increases the risk of death.” She added some tables from the supplemental material, showing the type of negative events and conditions that occurred. Her conclusion:
“In other words, any way you choose to look at it, no matter how carefully you slice and dice the data, there is simply no getting around the fact that homebirth increases the risk of perinatal death and brain damage.”
I guess the policy options might include include whether home births should be encouraged, more regulated, covered by public and/or private health insurance, banned, penalized or (further) stigmatized.
Home birth seems safer than letting children ride around unrestrained in the back of pickup trucks, which is legal in North Carolina – as long as they’re engaged in agricultural labor. On the other hand, we have helmet laws for kids on bicycles in many places. And if a child is injured in either situation, hopefully an ambulance would take them to the hospital even if the accident were preventable.
In other words, I don’t think policy questions can be resolved by a comparison of risks, however rigorous.