With the new PBS Frontline documentary Hunting the Nightmare Bacteria premiering this week, I hope that the American public is finally becoming aware of what many in the U.S. and around the world have seen coming for years. I encourage readers to check out the film and the links available online through PBS. However, I feel ethically bound to issue a ‘trigger warning’ for those who do not want to view a child and young adult being ravaged by diabolical infections.
Are we ready for the post-antibiotic era? Supposedly, we were all alerted last March when the CDC sounded an alarm – “Action needed now to halt spread of deadly bacteria” – but how many of us heard it?
We’re still in the dark when it comes to nightmare bacteria. At this point, I’m less convinced that anyone is “hunting” these antibiotic-resistant bacteria and more convinced that these microorganisms are hunting us. We need to be on the defensive, taking steps to protect ourselves, our loved ones, and our society.
Reading the PBS documentary’s link to “Eight Ways to Protect Yourself from Superbugs,” I found tips that are not new but are important reminders for public health. I’m a big believer in their recommendation to question the necessity and effectiveness of all prescriptions of antibiotics (e.g., that they cannot cure viral illnesses). That said, I’m sad that we still need to teach people how to properly wash their hands, and I’m even more dismayed that we have to recommend that everyone asks their medical providers to wash their hands. Unfortunately, promoting hand-washing is only a small improvement when proper drying methods are unavailable: studies continue to show that air hand dryers add more bacteria to clean hands.
In the documentary, Arjun Srinivasan, M.D., Associate Director of CDC, warns, “…the more antibiotics we put into people, we put into the environment, the more opportunities we create for these bacteria to become resistant….” However, the environmental components – government funding for research and surveillance, public health policies, and medical norms – are not fully addressed by this film. In addition, the causal link to meat and poultry policies/practices is completely absent. As a medical sociologist, my critique of this documentary is that it spends a lot of time on horrific case studies and too little time on the structural and social causes, consequences, and solutions to this crisis.
For a more complete picture, see the CDC’s report with graphics that illustrate the dynamics of drug resistance. I was stunned by chilling estimates: annually, antibiotic resistance will cause over 2 million Americans to become ill and will result in at least 23,000 deaths. In the early years of the HIV/AIDS epidemic, activists rallied public support and political action with the message that “Silence Equals Death” – what message will wake up Americans to the realities of our new nightmare?




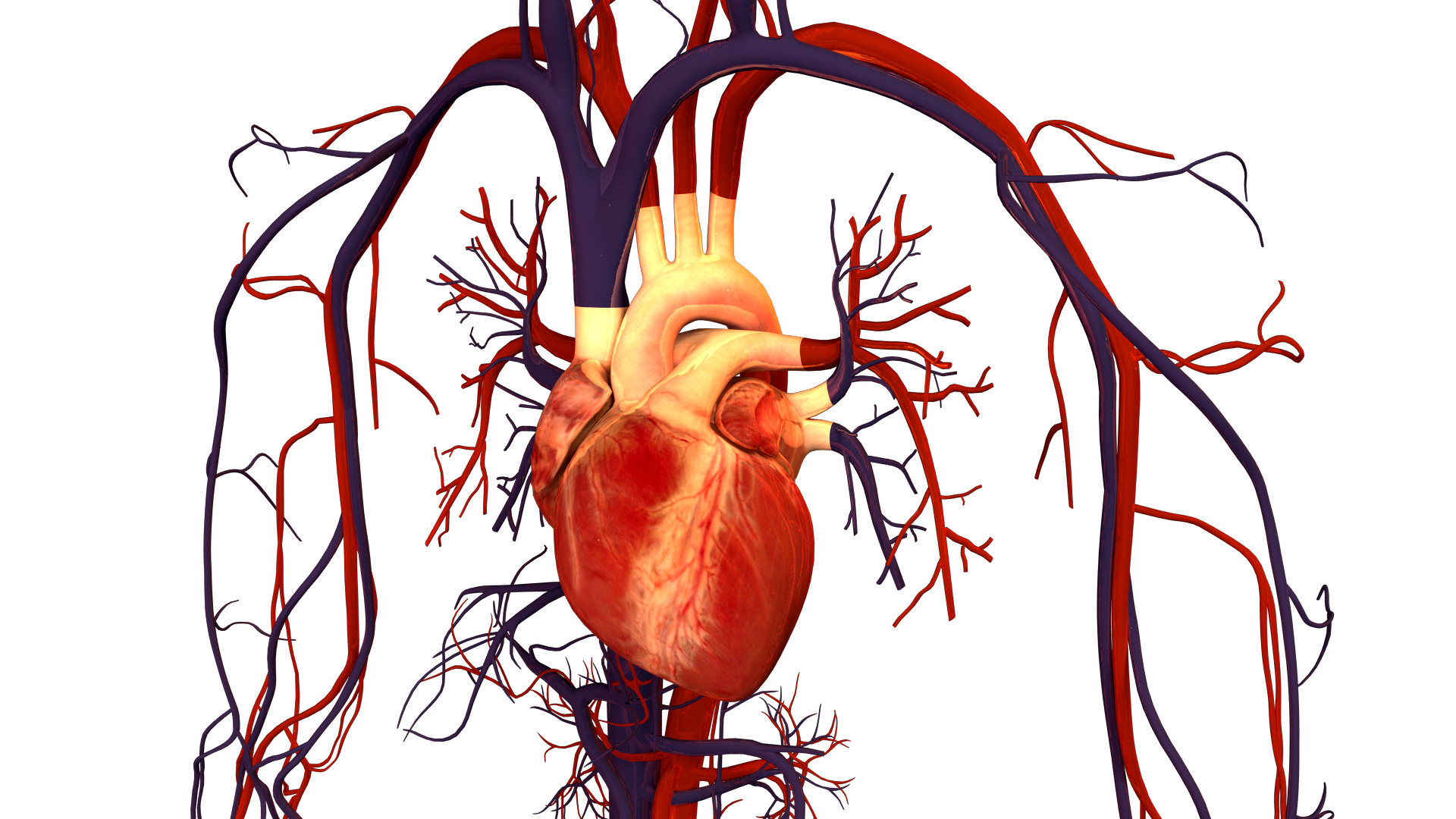 As a women’s health researcher, I am concerned about how long it is taking to bring attention and resources to this problem. After all, it has been decades since we’ve learned that cardiovascular disease affects women every bit as much–or even more–than it does men. Indeed, since 1984, cardiovascular disease has killed
As a women’s health researcher, I am concerned about how long it is taking to bring attention and resources to this problem. After all, it has been decades since we’ve learned that cardiovascular disease affects women every bit as much–or even more–than it does men. Indeed, since 1984, cardiovascular disease has killed 
