As a sexual health researcher, I have followed the saga of HPV (human papillomavirus) vaccination since the early 2000s. I’m posting this month’s column early to address three news stories that recently caught my attention – both for what they reported and also for what they left out:
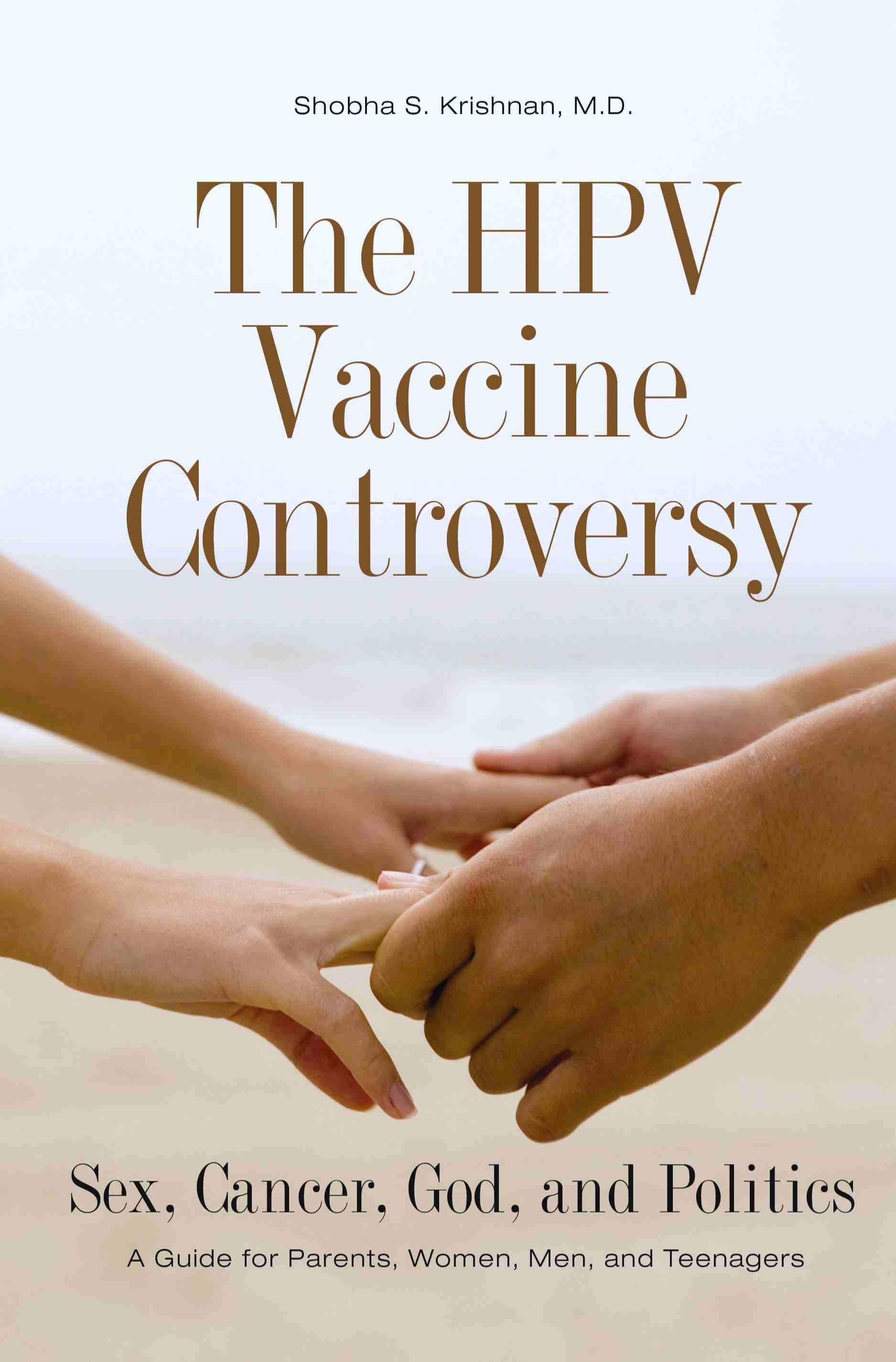
March 26, 2012: PRNewswire report on Harold zur Hausen’s remarks at the annual meeting of the Society of Gynecologic Oncology. Having won the 2008 Nobel Prize in Medicine for discovering the link between HPV and cervical cancer, zur Hausen kept the spotlight on cervical cancer when he advocated for HPV vaccination of young females and males in order to “eradicate cervical cancer.” While I advocated for non-sexist HPV vaccination policies back in a 2010 Ms. Magazine article, I was surprised by reports that zur Hausen favored male vaccination: “…if society were to vaccinate just one gender to prevent the spread of cervical-cancer causing HPV, it would be more effective to vaccinate just males.” I found myself asking two questions: (1) Why base medical recommendations on heterosexist assumptions that girls/women only contract cancer-causing strains of HPV from male partners? (2) Why continue to narrowly focus on HPV as a cause of cervical cancer, when a growing body of research documents its role in a range of genital cancers as well as often fatal oral-throat cancers?
April 2, 2012: The New York Times offers a summary of a study published in the March issue of the British Medical Journal: the findings suggest that HPV vaccination “can significantly cut the likelihood of virus-related disease even among women who have had surgery for cervical cancer caused by HPV.” The strongest prevention effect – 64% reduction in risk – was for women who had the most serious kinds of cervical cancer. The article quotes Dr. Elmar A. Joura, associate professor of gynecology at the Medical University of Vienna: “Regardless of your age or your history, a vaccination can prevent new disease.” Key question not addressed by this article: why does the CDC have an upper-age limit of 26 years old for HPV vaccination? Last year, Canada raised their upper-age limit to 45 – how much longer will ‘older’ Americans have to wait?
April 4, 2012: Forbes article on “The Gardasil Problem” fails to address the full scope of HPV vaccination ‘problems.’ First, the author misleads readers into thinking that HPV-related oral-throat cancers are “a new form” – again, see not only the 2010 Ms. Magazine article but also the Oral Cancer Foundation’s thorough summary of the decades of research linking sexually-transmitted HPV to serious oral cancers.
The author also misstates the focus/bias of Merck’s original years of marketing Gardasil: “When it was introduced in 2006…Merck began an advertising push to raise awareness of the risks of HPV.” What ads did he see? I and other consumers of mainstream media were exposed to a series of commercials that referred to Gardasil as “the cervical cancer vaccine” and strategically obscured message about “HPV-related diseases”, never clarifying for viewers that HPV was, in fact, sexually transmitted. While I offered a feminist critique of the branding and marketing of Gardasil in my 2008 book and several blog posts – trying to get the public to understand that “You don’t need to have a cervix to benefit from the cervical cancer vaccine” – Merck did not change to a focus on Gardasil as a STD vaccine until it received FDA approval for male vaccination…until profits depended upon bursting the bubble of the mythical cervical cancer vaccine.
Next, the author not only makes a heterosexist assumption but also unnecessarily demonizes oral sex on women as the ‘usual’ mode of transmission: “Usually transmitted when men perform oral sex on women, it can also spread through other forms of contact, perhaps even just kissing.” If kissing can transmit the virus, the why is he so sure that most of men with HPV-related oral-throat cancers skipped ‘first base’ and went straight to ‘third base’? If, and this is a big ‘if’, clinical studies can verify unprotected oral sex as the primary mode of transmission, then why not offer readers a brief education on the vaccine-free ways to practice safer oral sex?
Finally, the author unnecessarily dashes readers’ hopes for the near future: “tests that might well prove that [Gardasil] can prevent the new throat cancer strain would take at least 20 years, until the boys sampled actually became sexually active and then contracted the disease.” Why would these tests take 20 years? Does this author think that a boy who is vaccinated at age 12 will not perform oral sex until he’s 20+ years old? Where is the data to show it would take another ten years for HPV-related oral and throat cancers to develop? In addition, the author fails to point readers towards the likely source of delay: a lack of interest by the makers of the two FDA-approved HPV vaccines.
A 2010 article in the Journal of the National Cancer Institute not only clarifies the challenges of developing effective screening for oral HPV infections but also reports the truth about Merck’s failure to move forward with testing HPV vaccination as prevention of oral and throat cancers. Maura Gillison, M.D., Ph.D., a leading researcher on HPV-related head and neck cancers at Ohio State University in Columbus, explained why clinical trial plans were derailed in 2010: “We were 6 weeks from enrolling the first patient when I got an e-mail saying it was no longer in the interest of Merck to conduct the trial.” The article also quotes Pam Eisele, a Merck spokeswoman:
“The link between HPV infection and head and neck cancers continues to be an area of scientific interest for Merck; however, we currently do not have any plans to study the potential of Gardasil to prevent HPV-related oropharyngeal cancers. In 2008, we did conduct a small pilot study to assess our ability to obtain adequate and valid oropharyngeal samples. While the results of the pilot study were promising, due to competing research and business priorities we ultimately decided not to move ahead with an efficacy study at this time.”
Why is Forbes not asking for a more complete explanation of those “competing research and business priorities”? We, the American public, should demand more funding find out how to prevent cancers which research shows to be on the rise and more fatal than cervical cancer in the U.S.
The one section of this Forbes article that some readers might find valuable is its summary of the data on the safety record of HPV vaccination. However, as I’ve said before, I am not advocating that vaccination is the only way to reduce one’s risk of contracting cancer-causing strains of HPV. Those who decide not to vaccinate themselves and/or their children need to learn the facts about HPV prevention, testing, diagnosis, and treatment: check out the American Social Health Association’s online HPV and Cervical Cancer Prevention Resource Center.


 In light of the new Pap smear guidelines, I hope that U.S. girls and women who get less frequent Pap tests will more frequently ask their healthcare practitioners to educate them about
In light of the new Pap smear guidelines, I hope that U.S. girls and women who get less frequent Pap tests will more frequently ask their healthcare practitioners to educate them about